Study population
The Japan Public Health Center-Based Prospective Study (JPHC Study) is a prospective study performed using a population-based sample of 140,420 Japanese adults (68,722 men and 71,698 women) in two cohorts based on public health centre (PHC) areas: Cohort I (started in 1990, five PHC areas) and Cohort II (started in 1993, six PHC areas).
The residents of these 11 PHC areas were identified through population registries managed by local municipalities. A previous study has presented the details of the JPHC Study protocol23. Since participants from the Tokyo and Osaka areas were excluded from the present study due to unavailable incidence data, 116,896 participants (57,713 men and 59,183 women) from nine PHC areas were considered eligible for follow-up. Informed consent was obtained from each participant implicitly when they completed the baseline questionnaire, where the study purpose and follow-up procedures were described. This study followed the tenets of the Declaration of Helsinki and was approved by the institutional review boards of Azabu University, Toyo University, and the National Cancer Center, Tokyo, Japan.
A self-administered questionnaire was distributed to all residents in the study areas for Cohorts I and II. The questionnaire included items that captured demographic characteristics, medical history, smoking and drinking habits, and a simplified version of dietary habits. A 5-year follow-up survey was conducted for Cohort I in 1995 and Cohort II in 1998 using a questionnaire that included items regarding irregular routine in daily life and demographic characteristics, in addition to a more comprehensive food frequency questionnaire (FFQ). Therefore, we used these questionnaires as the starting point to assess the association between irregular daily routine and CVD incidence risk.
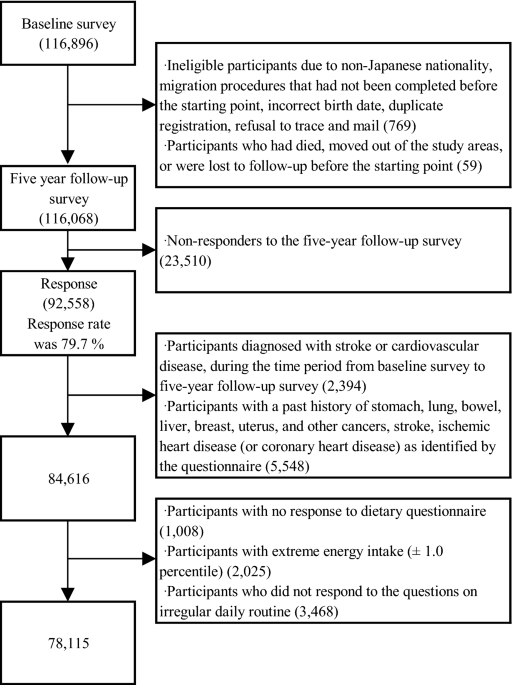
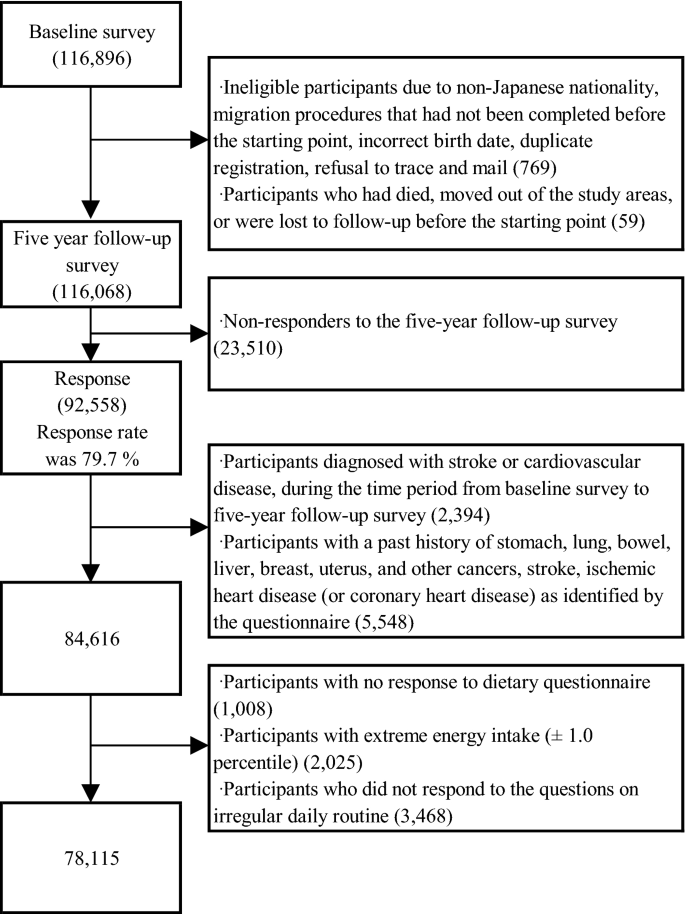
We excluded participants with non-Japanese nationality, migration procedures that had not been completed before the starting point, incorrect birth date, duplicate registration, and those who refused follow-up, died, moved out of the study areas, or were lost to follow-up before the starting point. Finally, 116,068 participants were eligible for this study. Among them, 92,558 participants responded to the 5-year follow-up questionnaire, yielding a response rate of 79.7%, and were included. Among these participants, we excluded those who were diagnosed with CVD in the period from the baseline survey to the 5-year follow-up survey (n = 2394) and those who had a past history of cancer (e.g. stomach, lung, bowel, liver, breast, uterine cancer, or other cancers), stroke, and ischaemic heart disease (or coronary heart disease [CHD]), as identified by the questionnaire (n = 5548). Furthermore, 1008 participants who did not complete the diet section of the questionnaire, 2025 participants with extreme total energy intake (lower and upper 1.0 percentile for men and women: 785 and 5096 kcal/day, and 656 and 4472 kcal/day, respectively), and 3468 participants who did not respond to the questions on irregular daily routine were excluded. Finally, 78,115 participants (36,210 men and 41,905 women) were included in the statistical analyses (Fig. 1).
Assessment of irregular daily routine and dietary intake
The self-reported irregular daily routine was assessed by the response to the question, ‘Is your daily routine or activity schedule regular?’ in the questionnaire. The possible response to this question was ‘yes’ or ‘no’. Participants who responded with ‘no’ were considered to have an irregular daily routine; participants who responded with ‘yes’ were included as the reference group. Dietary intake was assessed using the FFQ, consisting of 138 food and beverage items. The 5-year follow-up questionnaire was based on nine frequency categories (‘almost never’ to ‘seven or more times per day’) for vegetables and fruits and nine frequency choices (‘almost never’ to ‘10 or more glasses per day’) for juices. Standard portion sizes for each food item were categorised as follows: small (50% smaller than standard), medium (same as standard), and large (50% larger than standard). The quantity (g/day) of consumed vegetables and fruits was calculated from the data obtained. The FFQ for assessing vegetable and fruit consumption has already been validated in previous studies24,25.
Potential confounding factors
Potential confounding factors included age, sex, body mass index (BMI) (quartile), smoking status (never smoker, ex-smoker, or current smoker), sleep duration (6–8 h/day, ≤ 5 h/day, ≥ 9 h/day), breakfast (eating every day or other frequencies), working hours, perceived mental stress (low, medium, or high), living arrangement (living alone or others), job type (agriculture, forestry, fishery, or self-employed; salaried or professional; housework or unemployed), study area, alcohol intake (0, 1–150, 150–300, or ≥ 301 g/week), quartiles of metabolic equivalent task-hours per day (METs), total energy intake, vegetable, fruit, fish, meat, and sodium intake. The consumption of each food group was adjusted by the total energy intake using the residual method26.
Follow-up survey
Participants in Cohorts I and II were followed from 1995 to December 31, 2009, and from 1998 to December 31, 2012, respectively. Information about any changes in residence status was obtained annually from data on moving out of the area, identified by residency registration inside and outside the PHC areas. All mortality data of participants in the residential registry were forwarded to the Ministry of Health, Labour and Welfare and were coded for inclusion in the National Vital Statistics. Since residency and death registrations are required by the Basic Resident Registration Law and Family Registration Law, respectively, data from each registration were considered complete.
Ascertainment of stroke and CHD incidence
The medical records were reviewed by hospitals or PHC physicians in each registered major hospital within the PHC areas27,28. Diagnoses of stroke were based on focal neurologic symptoms and confirmed using computed tomography scan and/or magnetic resonance imaging according to the criteria of the National Survey of Stroke29. Diagnoses of myocardial infarction were confirmed in the medical records according to the criteria of the MONICA project30. Sudden cardiac death was defined as death of unknown origin that occurred within 1 h of the onset of the event. These medical data were extracted according to cohort-specific registration forms.
For the analyses, only the first-ever CVD events during the follow-up were regarded as incident CVD. If one person suffered both stroke and CHD, CVD was defined, whichever occurred first. Person-years of follow-up were calculated for each participant from baseline to the date of death, diagnosis, emigration from the PHC area, or end of the follow-up period (December 31, 2009, or December 31, 2012), whichever occurred first. Participants lost to follow-up were censored at the last confirmed date of their presence in the PHC area. A total of 1,038,087 person-years for the CVD analysis was accrued.
Statistical analysis
All statistical analyses were divided by sex, and the participants were divided into two groups according to their daily routine: the regular and irregular groups. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated using the Cox proportional hazards model, according to the SAS PHREG Procedure (SAS Institute, Inc., Cary, NC, USA). Multivariable Cox regression models with a covariate adjustment approach were used: model l included age at baseline and study area; model 2 included model 1 plus covariates, including living arrangement (living alone, other, or missing), alcohol intake (0, 1–150, 151–300, 301–450, and ≥ 451 g/week), cigarette smoking status (current [< 20 or ≥ 20 cigarettes/day], never, former, or missing), perceived mental stress (low, medium, high, or missing), working hours (< 5 h, ≥ 5 h and < 9 h, ≥ 9 h, or missing), job type (agriculture, forestry, fishery, and self-employed; office work, profession, and other work; housework and unemployed; or missing), breakfast (eating every day, other frequencies, or missing), sleep duration (≤ 5 h, ≥ 6 h and ≤ 8 h, ≥ 9 h, or missing), quartile of BMI, METs, and dietary factors (i.e. quartiles of energy intake and energy-adjusted dietary intakes of vegetables, fruits, meat, fish, and sodium). Missing covariate data were adjusted using dummy variables. Since hypertension, hypercholesterolaemia, and diabetes mellitus could be considered potential mediators of the association between an irregular daily routine and the increased risk of CVD, we included multivariable analysis data concerning the medication use for hypertension, hypercholesterolaemia, and diabetes mellitus in Table S1.
Since a significant inverse association between vegetable and fruit consumption and CVD risk has been reported22, we further explored the interaction between an irregular daily routine and vegetable and fruit consumption (dichotomised variable) on CVD risk by adding cross-product terms into the multivariable model. Moreover, stratified analyses according to selected demographic characteristics (i.e. BMI, living arrangement, smoking and drinking habits, working hours, type of job, total physical activity, perceived mental stress, sleep duration, and skipping breakfast) were also conducted to determine the heterogeneity of association between an irregular daily routine and CVD risk. A two-tailed p-value of < 0.05 was considered statistically significant.
Ethics approval and consent to participate
Informed consent was obtained from each participant implicitly when they completed the baseline questionnaire, where the study purpose and follow-up procedures were described. The study protocol was approved by the institutional review boards of Azabu University, Toyo University, and the National Cancer Center, Tokyo, Japan.